Introduction
Know more about PSA tests
What you need to know about MRI Scans
What is prostate biopsy
Start a prostate risk test now
Overview of Prostate tests
The purpose of prostate cancer screening is to detect tumors before they spread. Prostate cancer diagnoses should be made as early as feasible to improve prostate outcomes because African men experience more aggressive disease than their Caucasian counterparts.
However, some medical advocates advise that African men start talking to their doctors about prostate cancer screening once they age 40. In general, the guidelines propose that men begin screening for prostate cancer after 50 years.
Your doctor might inquire about potential sexual and urogenital issues, including their duration and frequency. Your doctor will typically conduct a physical examination and/or blood test to assess your prostate’s condition if he fears you have prostate cancer.
PSA Tests
What is a Prostate-Specific Antigen (PSA)?
Prostate-specific antigen, or PSA, is a protein produced by normal, malignant, cells of the prostate gland. The PSA test measures the level of PSA in a man’s blood. For this test, a blood sample is sent to a laboratory for analysis. The results are usually reported as nanograms of PSA per milliliter (ng/mL) of blood.
Why would I need this test?
PSA test is used to screen for prostate cancer. Screening is a test that looks for a disease, such as cancer, in its early stages, when it’s most treatable. Therefore you may get a PSA test if you have certain risk factors for prostate cancer. These include:
- Men with a family history of prostate cancer
- Your age: Prostate cancer is more common in men over the age of 50.
- Being African: Prostate cancer is more common in African men. The reason for this is unknown.
You may also get a PSA test if:
- You have symptoms such as painful or frequent urination, and pelvic and/or back pain.
- You’ve already been diagnosed with prostate cancer. The PSA test can help monitor the effects of your treatment.
How do I prepare for a PSA test?
If our doctors requests that you should have a PSA test, make sure that they are aware of any prescription or medicines, vitamins, or supplements you take. Certain drugs may cause the test results to be falsely low.
If our doctors thinks your medication might interfere with the results, they may decide to request a different test or they may ask you to avoid taking your medicine for several days so your results will be more accurate.
How is a PSA performed?
- You are required to sit upright in a chair and rest your arm face up on an elevated arm rest. The will tie a strap (tourniquet) around the top of your arm to temporarily restrict the blood flow from your arm back to your heart. This will make the vein inside your elbow “pop out”, and therefore easier to find. The area where the needle will be inserted is wiped with a sterile alcohol wipe to reduce any risk of infection. A needle is inserted into the vein and a small amount of blood is drawn into the vial attached to the needle.
- If seeing blood makes you uneasy, it is best to look away. Usually the phlebotomist will ask you questions as they take the blood to distract you from the procedure. It is done in no time! If there is any pain at all, it is minimal. More often than not, you will only feel a slight discomfort.
- After the procedure, the phlebotomist will press a small wad of cotton on the entry point to stop the flow of blood. The cotton wad is strapped on with a band aid. This only needs to remain on for a couple of hours. Sometimes a little bruise is left in this spot, but this is nothing to worry about.
What do the results of my PSA test mean?
In general, a PSA level that is above 4.0 ng/mL is considered suspicious. However, there are many other factors to consider before taking further action. The following are some general PSA level guidelines:
- 0 to 2.5 ng/mL is considered safe
- 6 to 4 ng/mL is safe in most men but talk with our doctors about other risk factors
- 0 to 10.0 ng/mL is suspicious and might suggest the possibility of prostate cancer. It is associated with a 25% chance of having prostate cancer.
- 0 ng/mL and above is dangerous and should be discussed with our doctors immediately. It is associated with a 50% chance of having prostate cancer.
If Your PSA is High
Talking to our doctors can explore several options if your PSA is high. One option is to have a second PSA screening; recent research has shown that a second screening can improve the accuracy of an abnormal result. A digital rectal exam (DRE) and a biopsy can also confirm the presence or absence of prostate cancer. However, there are several other reasons why a PSA result might be high:
- Advanced age
- Recent biopsy
- Catheter
- Injury to pelvic region or prostate
- Prostatitis
- Riding a bicycle
- Sex (within the past 24 hours)
- Supplements that effect testosterone
- Urinary tract infection
If Your PSA is Rising Quickly
The rate in yearly increase in the PSA level is known as the PSA velocity. This is one measure of prostate cancer risk, since PSA levels can rise rapidly in men who have prostate cancer. This can be especially useful to find prostate cancer in early stages before the cancer has left the capsule of the prostate.
PSA result between 4.0 and 10.0 ng/ml is an early indicator of prostate cancer if a man.
>What are the risks of a PSA test?
Drawing blood is considered safe. However, because veins and arteries vary in size and depth, getting a blood sample is not always simple.
The healthcare professional who draws your blood may have to try several veins in multiple locations on your body before they find one that allows them to get enough blood.
Drawing blood also has several other risks. These include risk of:
- Fainting
- Excessive bleeding
- Feeling lightheaded or dizzy
- An infection at the puncture site
- A hematoma, or blood collected under the skin, at the puncture site.
References:


Common problems arising after prostate cancer surgery
Magnetic resonance imaging (MRI) is a type of scan that uses strong magnetic fields and radio waves to produce detailed images of the inside of the body.
The MRI scanner causes no pain. If a person is awake during the test, the person may feel some discomfort or pressure when the needle is inserted. An MRI scan may not be possible if you have a pacemaker or other metal inside your body.
Pros and Cons of MRI Scan Before Biopsy
Advantages
- It can give your doctor information about how likely it is that you have cancer in your prostate.
- It’s less likely than a biopsy to pick up a slow-growing cancer. This means you are less likely to have a biopsy and treatments that could have life-changing side effects if your cancer is unlikely to cause you any problems in your lifetime. Some side effects include severe infections and long lasting urinary or sexual problems.
- It can help your doctor decide if you need a biopsy – if there’s nothing unusual on the scans, this means you’re unlikely to have prostate cancer that needs to be treated. You may be able to avoid having a biopsy, and its possible side effects.
- If you do need a biopsy, your doctor can use the scan images to decide which parts of the prostate to take samples from.
- If your biopsy finds cancer, you probably won’t need another scan to check if it has spread, as the doctor can get this information from your first MRI scan. This means you can start talking about suitable treatments as soon as you get your biopsy results.
Disadvantages
- Being in the MRI machine can be unpleasant if you don’t like closed or small spaces (claustrophobia).
- Some men are given an injection of dye during the scan – this can sometimes cause mild side effects.
What does an MRI scan involve?
Before the scan the doctor or nurse will ask questions about your health. As the scan uses magnets, they will ask whether you have any metal in your body such as implants or fragments that could be attracted to the magnet. They will decide if you can't have an MRI or if there are any changes needed to make sure the MRI is as safe as possible for you. For example, if you have a pacemaker for your heart you may not be able to have an MRI scan. You’ll also need to take off any jewellery or metal items. If you use patches on your skin such as pain medication, you should ask the doctor if this should be removed for the MRI scan.
You will lie very still on a table, which will move slowly into the scanner which is shaped like a doughnut or a long tunnel. If you don’t like closed or small spaces (claustrophobia), tell your radiographer (the person who takes the images) and they may be able to suggest some ways that could help you feel more comfortable in the scanner.
The radiographer might give you an injection of a dye during the scan. The dye helps them see the prostate and other organs more clearly on the scan. It is usually safe, but can sometimes cause problems if you:
- have kidney problems
- have asthma
- are allergic to the dye or have any other allergies.
Let the radiographer know if you have either of these.
The scan takes 30 to 40 minutes. The machine won’t touch you but it is very noisy and you might feel warm. The radiographer will leave the room but you’ll be able to speak to them through an intercom, and will wear earplugs or ear defenders. You may also be able to listen to music through headphones.
Getting the results
Your MRI scan images will be looked at by a specialist called a radiologist, who specialises in diagnosing health problems using X-rays and scans. The radiologist will give the images of your prostate a score from 1 to 5. You may hear this called your PI-RADS (Prostate Imaging – Reporting and Data System) score or your Likert score. It tells your doctor how likely it is that you have cancer inside your prostate.
PI-RADS and Likert scores have the same values, and your score will be between 1 and 5.
- PIRADS or Likert score 1 It’s very unlikely that you have prostate cancer that needs to be treated
- PIRADS or Likert score 2 It’s unlikely that you have prostate cancer that needs to be treated.
- PIRADS or Likert score 3 It isn’t possible to tell from the scan whether you have prostate cncer that needs to be treated – you may hear this called a borderline result.
- PIRADS or Likert score 4 It’s likely that you have prostate cancer that needs to be treated.
- PIRADS or Likert score 5 It’s very likely that you have prostate cancer that needs to be treated.
If your PI-RADS or Likert score is 1 or 2
This means you’re unlikely to have prostate cancer that needs to be treated. Your doctor would discuss advantages and disadvantages of having a further biopsy to help make a shared decision with you. This would include talking through your individual risk factors such as age, ethnicity or family history.
Together, you and your doctor may decide that you don’t need to have a biopsy. Your doctor may suggest you have regular PSA tests so that any changes in your PSA level are picked up early. You’ll also be offered treatment for any urinary symptoms.
Or you and your doctor can decide for you to have a prostate biopsy as it will help confirm if there is no cancer that needs to be treated.
If your PI-RADS or Likert score is 3 or more
You’ll usually be offered a prostate biopsy to find out whether you have cancer.
References:



What can help with leaking urine?
There are treatments and products available that can help, and there are things you can do to help yourself. Your treatment options will depend on how much urine you’re leaking, and how recently you had your prostate cancer treatment.
Treatments and products available that can help include:
absorbent pads and pants
pelvic floor muscle exercises
urinary sheaths
bed protectors and handheld urinals
penile clamps.
If you have sudden urges to urinate (urinary urgency) and sometimes leak urine before you get to the toilet (urge incontinence), you may be offered bladder retraining.
If you still leak urine six to twelve months after surgery and pelvic floor muscle exercises haven’t helped, there are treatments available that might help. These may include:
an internal male sling
an artificial urinary sphincter
adjustable balloons
medicines.
Talk to your doctor or nurse about treatments and products that may be suitable for you.
Absorbent pads and pants
These can be worn inside your underwear or instead of underwear to soak up any leaks. Some people find it helpful to wear close fitting underwear with pads. You may want to try female pads as your leaking improves, as these tend to be smaller and lighter and may fit better. Pads are usually very discreet, so people won’t know you’re wearing them. But you may feel more confident wearing dark trousers so it won’t show as much if your pad does leak.
Services vary from area to area, but your GP or the continence nurses at your hospital may provide some pads for free. Or you can buy them in supermarkets, chemists or online. Age UK also has a range of products that can be ordered online.
If you haven’t had your operation yet, you might find it helps to prepare by finding out what products are available. Talk to your doctor, nurse or continence advisor for more information, or visit the Continence Product Advisor website.
Pelvic floor muscle exercises
These can strengthen the pelvic floor muscles, which help control when you urinate.
Read about pelvic floor muscle exercises.
Urinary sheaths
You might hear these called external catheters. These look like condoms with a tube attached to the end that drains urine into a bag. The sheath fits tightly over the penis and you can strap the bag to your leg – under your clothes – and empty it as needed.
Bed protectors and handheld urinals
If you have to go to the toilet often during the night, or you leak urine when you’re in bed, bed protectors or handheld urinals might be useful to you.
Bed protectors are large pads that protect your sheets and mattress by soaking up any urine that you might leak. There are pads that you can wash and reuse, and others that you only use once before throwing them away
Handheld urinals are containers with a lid that can be used if you can’t reach the toilet in time or if there isn’t a toilet nearby. They have a large opening with a lid so that you can store the urine until you reach a toilet. These might also be useful if you drive long distances and don’t have any toilet near you.
Penile clamps
A penile clamp fits onto the penis and squeezes it, closing the urethra so that no urine can leak out. You should only use a penile clamp during the day for short periods of time, and should open it at least every two hours to let your blood flow back into your penis.
A penile clamp fits onto the penis and squeezes it, closing the urethra so that no urine can leak out. You should only use a penile clamp during the day for short periods of time, and should open it at least every two hours to let your blood flow back into your penis.
Penile clamps can be uncomfortable to wear and aren’t commonly used in the UK. They aren’t usually recommended by health professionals, as they reduce the blood flow to the penis. This means it can be unsafe if a clamp is put on too tightly or for too long. However, some men like to use them for activities such as swimming or jogging.
For more information about the different types of products to manage leaking urine, visit Continence Product Advisor.
Internal male sling
This is a small piece of material (mesh) that presses gently on your urethra and supports the urinary sphincter to keep it closed. This helps to stop urine leaking. You’ll have an operation to fit the sling. It should be tight enough to stop urine leaking out, but loose enough to let you urinate when you want to.
About prostate biopsy
Biopsy is an examination of tissue removed from a living body to discover the presence, cause, or extent of a disease. just because your doctor orders a biopsy, it doesn’t mean that you have cancer. Doctors use biopsies to test whether abnormalities in your body are caused by cancer or by other conditions. A prostate biopsy is a procedure to remove samples of suspicious tissue from the prostate using a thin needle to take small samples of tissue from the prostate.
There are two main types of prostate biopsy:
Talk to your doctor or nurse about whether you will have a TRUS biopsy or a transperineal biopsy.
In many hospitals you may have a special type of magnetic resonance imaging (MRI) scan, called a multi-parametric MRI (mpMRI) scan, before having a biopsy. In other hospitals you may have a biopsy first.
What are the advantages and disadvantages of having a biopsy?
Your doctor should talk to you about the advantages and disadvantages of having a biopsy. If you have any concerns, discuss them with your doctor or specialist nurse before you decide whether to have a biopsy.
Advantages
- It’s the only way to find out for certain if you have cancer inside your prostate.
- It can help find out how aggressive any cancer might be – in other words, how likely it is to spread.
- It can pick up a faster growing cancer at an early stage, when treatment may prevent the cancer from spreading to other parts of the body.
- If you have prostate cancer, it can help your doctor or nurse decide which treatment options may be suitable for you.
- If you have prostate cancer, you’ll usually need to have had a biopsy if you want to join a clinical trial in the future. This is because the researchers may need to know what your cancer was like when it was first diagnosed.
Disadvantages
- The biopsy can only show whether there was cancer in the samples taken, so it’s possible that cancer might be missed.
- It can pick up a slow growing or non-aggressive cancer that might not cause any symptoms or problems in your lifetime. You would then have to decide whether to have treatment or to have your cancer monitored. Having your cancer monitored rather than having treatment may make you worry about your cancer. But having treatment can cause side effects that can be hard to live with. The knowledge of having a slow growing or non-aggressive cancer affects everyone differently and there is no right or wrong way to feel.
- A biopsy has side effects and risks, including the risk of getting a serious infection.
- If you take medicines to thin your blood, you may need to stop taking them for a while, as the biopsy can cause some bleeding for a couple of weeks.
What does a prostate biopsy involve?
If you decide to have a biopsy, you’ll either be given an appointment to come back to the hospital at a later date or offered the biopsy straight away.
Before the biopsy you should tell your doctor or nurse if you’re taking any medicines, particularly antibiotics or medicines that thin the blood such as warfarin or aspirin.
You may be given some antibiotics to take before your biopsy, either as tablets or an injection, to help prevent infection. You might also be given some antibiotic tablets to take at home after your biopsy. It’s important to take them all so that they work properly.
A doctor or nurse will do the biopsy. There are two main types of biopsy:
- a trans-rectal ultrasound (TRUS) guided biopsy, where the needle goes through the wall of the back passage
- a transperineal biopsy, where the needle goes through the skin between the testicles and the back passage (the perineum).
The type of biopsy you will have depends on your hospital.
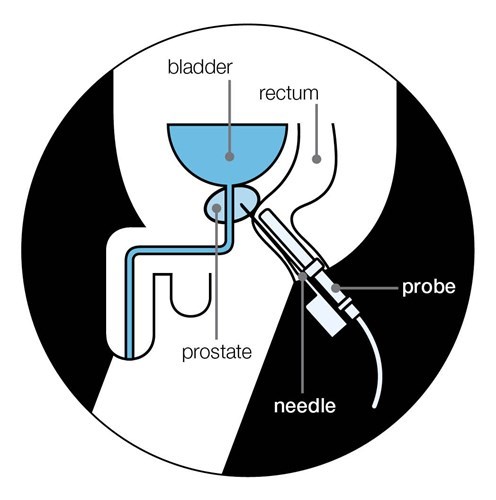
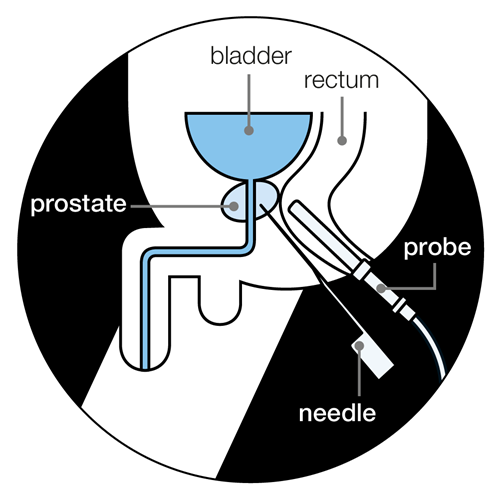
What is a TRUS biopsy?
The doctor or nurse uses a thin needle to take small samples of tissue from the prostate through the wall of the back passage (rectum).
You’ll lie on your side on an examination table, with your knees brought up towards your chest. The doctor or nurse will put an ultrasound probe into your back passage (rectum), using a gel to make it more comfortable. The ultrasound probe scans the prostate and an image appears on a screen. The doctor or nurse uses this image to guide where they take the cells from. If you’ve had an MRI scan, the doctor or nurse may use the images to decide which areas of the prostate to take biopsy samples from.
You will have an injection of local anaesthetic to numb the area around your prostate and reduce any discomfort. The doctor or nurse then puts a needle next to the probe in your back passage and inserts it through the wall of the back passage into the prostate. They usually take 10 to 12 small pieces of tissue from different areas of the prostate. But, if the doctor is using the images from your MRI scan to guide the needle, they may take fewer samples.
The biopsy takes 5 to 10 minutes. After your biopsy, your doctor may ask you to wait until you've urinated before you go home. This is because the biopsy can cause the prostate to swell, so they'll want to make sure you can urinate properly before you leave. You should ask your doctor or nurse if you need to get someone to take you home or if you can drive yourself home.
What is a transperineal biopsy?
This is where the doctor inserts the biopsy needle into the prostate through the skin between the testicles and the back passage (perineum).
A transperineal biopsy can be done under either general anaesthetic or local anaesthetic. If you have a biopsy under general anaesthetic, you will be asleep and won’t feel anything. A general anaesthetic can cause side effects – your doctor or nurse should explain these before you have your biopsy.
If you have a biopsy using a local anaesthetic, you are awake during the procedure and the anaesthetic numbs the prostate and the area around it.
The doctor will put an ultrasound probe into your back passage, using a gel to make this easier. An image of the prostate will appear on a screen, which will help the doctor to guide the biopsy needle.
There are two main types of transperineal biopsy you may have:
A targeted transperineal biopsy
This is where the doctor may just take a few samples from the area of the prostate that looked usual on the scan images from your MRI.
A template transperineal biopsy
This is where the doctor places a grid (template) over the area of skin between the testicles and back package. They then insert the needle though holes in the grid, into the prostate. They might take up to 25 or more samples from different areas of the prostate. A template biopsy is sometimes used if a TRUS biopsy hasn’t found any cancer, but the doctor still thinks there might be cancer.
You will need to wait a few hours to recover from the anaesthetic before going home. You should ask your doctor or nurse if you need to get someone to take you home or if you can drive yourself home.
A transperineal biopsy usually takes about 20 to 40 minutes. You will need to wait a few hours to recover from the anaesthetic before going home. You should ask your doctor or nurse if you need to get someone to take you home or if you can drive yourself home. Your doctor may ask you to wait until you’ve urinated. This is because the biopsy can cause the prostate to swell, so they’ll want to make sure you can urinate properly before you leave.
What are the side effects of a biopsy?
Having a biopsy can cause side effects. These will affect each man differently, and you may not get all of the possible side effects.
Pain or discomfort
Some men feel pain or discomfort in their back passage (rectum) for a few days after a TRUS biopsy. Others feel a dull ache along the underside of their penis or lower abdomen (stomach area). If you have a transperineal biopsy, you may get some bruising and discomfort in the area where the needle went in for a few days afterwards.
If you receive anal sex, wait about two weeks, or until any pain or discomfort from your biopsy has settled, before having sex again. Ask your doctor or nurse at the hospital for further advice.
Some men find the biopsy painful, but others have only slight discomfort. Your nurse or doctor may suggest taking mild pain-relieving drugs, such as paracetamol, to help with any pain.
If you have any pain or discomfort that doesn’t go away, talk to your nurse or doctor.
Short-term bleeding
It’s normal to see a small amount of blood in your urine or bowel movements for about two weeks. You may also notice blood in your semen for a couple of months – it might look red or dark brown. This is normal and should get better by itself. If it takes longer to clear up, or gets worse, you should see a doctor straight away.
A small number of men who have a TRUS biopsy may have more serious bleeding in their urine or from their back passage (rectum). This can also happen if you have a transperineal biopsy but it isn't very common. If you have severe bleeding or are passing lots of blood clots, this is not normal. Contact your doctor or nurse at the hospital straight away, or go to the accident and emergency (A&E) department at the hospital.
Infection
Some men get an infection after their biopsy. This is more likely after a TRUS biopsy than after a transperineal biopsy. It's very important to take any antibiotics you’re given, as prescribed, to help prevent this. But you might still get an infection even if you take antibiotics.
Symptoms of a urine infection may include:
- pain or a burning feeling when you urinate
- dark or cloudy urine with a strong smell
- needing to urinate more urgently than usual
- needing to urinate more often than usual during the day or night
- a high or very low temperature
- pain in your lower abdomen (stomach area) or back.
If you have any of these symptoms, contact your doctor or nurse at the hospital straight away. If you can’t get in touch with them, call your GP.
Less than 1 in 100 men (one per cent) who have a TRUS biopsy get a more serious infection that requires going to hospital. If the infection spreads into your blood, it can be very serious. This is called sepsis. Symptoms of sepsis may include:
- a high temperature (fever)
- chills and shivering
- blue, pale or blotchy skin, lips or tongue
- a fast heartbeat
- fast breathing or difficulty breathing
- confusion or changes in behaviour.
If you have symptoms of sepsis, go to your nearest hospital A&E department straight away.
Acute urine retention
A small number of men find they suddenly and painfully can’t urinate after a biopsy – this is called acute urine retention. This happens because the biopsy can cause the prostate to swell, making it difficult to urinate. Acute urine retention may be more likely if you have a template biopsy. This is because more samples are taken, so there may be more swelling.
Your doctor will make sure you can urinate before you go home after your biopsy. If you can’t urinate, you might need to have a catheter for a few days at home – this is a thin tube that’s passed into your bladder to drain urine out of the body.
If you develop acute urine retention at home, contact your doctor or nurse at the hospital straight away, or go to your nearest A&E department. You might need a catheter for a few days.
Sexual problems
You can masturbate and have sex after a biopsy. If you have blood in your semen, you might want to use a condom until the bleeding stops.
A small number of men have problems getting or keeping an erection (erectile dysfunction) after having a biopsy. This may happen if the nerves that control erections are damaged during the biopsy. It isn’t very common and it should get better over time, usually within two months. Speak to your doctor or nurse if you’re worried about this.
What do my biopsy results mean?
The biopsy samples will be looked at under a microscope to check for any cancer cells. Your doctor will be sent a report, called a pathology report, with the results. The results will show whether any cancer was found. They may also show how many biopsy samples contained cancer and how much cancer was present in each sample.
It can take up to two weeks to get the results of the biopsy, but it can take longer in some hospitals. Ask your doctor or nurse when you're likely to get the results. You might be sent a copy of the pathology report. And you can ask to see copies of letters between the hospital and your GP. If you have trouble understanding any of the information, ask your doctor to explain it or speak to our Specialist Nurses.



What can help with leaking urine?
There are treatments and products available that can help, and there are things you can do to help yourself. Your treatment options will depend on how much urine you’re leaking, and how recently you had your prostate cancer treatment.
Treatments and products available that can help include:
absorbent pads and pants
pelvic floor muscle exercises
urinary sheaths
bed protectors and handheld urinals
penile clamps.
If you have sudden urges to urinate (urinary urgency) and sometimes leak urine before you get to the toilet (urge incontinence), you may be offered bladder retraining.
If you still leak urine six to twelve months after surgery and pelvic floor muscle exercises haven’t helped, there are treatments available that might help. These may include:
an internal male sling
an artificial urinary sphincter
adjustable balloons
medicines.
Talk to your doctor or nurse about treatments and products that may be suitable for you.
Absorbent pads and pants
These can be worn inside your underwear or instead of underwear to soak up any leaks. Some people find it helpful to wear close fitting underwear with pads. You may want to try female pads as your leaking improves, as these tend to be smaller and lighter and may fit better. Pads are usually very discreet, so people won’t know you’re wearing them. But you may feel more confident wearing dark trousers so it won’t show as much if your pad does leak.
Services vary from area to area, but your GP or the continence nurses at your hospital may provide some pads for free. Or you can buy them in supermarkets, chemists or online. Age UK also has a range of products that can be ordered online.
If you haven’t had your operation yet, you might find it helps to prepare by finding out what products are available. Talk to your doctor, nurse or continence advisor for more information, or visit the Continence Product Advisor website.
Pelvic floor muscle exercises
These can strengthen the pelvic floor muscles, which help control when you urinate.
Read about pelvic floor muscle exercises.
Urinary sheaths
You might hear these called external catheters. These look like condoms with a tube attached to the end that drains urine into a bag. The sheath fits tightly over the penis and you can strap the bag to your leg – under your clothes – and empty it as needed.
Bed protectors and handheld urinals
If you have to go to the toilet often during the night, or you leak urine when you’re in bed, bed protectors or handheld urinals might be useful to you.
Bed protectors are large pads that protect your sheets and mattress by soaking up any urine that you might leak. There are pads that you can wash and reuse, and others that you only use once before throwing them away
Handheld urinals are containers with a lid that can be used if you can’t reach the toilet in time or if there isn’t a toilet nearby. They have a large opening with a lid so that you can store the urine until you reach a toilet. These might also be useful if you drive long distances and don’t have any toilet near you.
Penile clamps
A penile clamp fits onto the penis and squeezes it, closing the urethra so that no urine can leak out. You should only use a penile clamp during the day for short periods of time, and should open it at least every two hours to let your blood flow back into your penis.
A penile clamp fits onto the penis and squeezes it, closing the urethra so that no urine can leak out. You should only use a penile clamp during the day for short periods of time, and should open it at least every two hours to let your blood flow back into your penis.
Penile clamps can be uncomfortable to wear and aren’t commonly used in the UK. They aren’t usually recommended by health professionals, as they reduce the blood flow to the penis. This means it can be unsafe if a clamp is put on too tightly or for too long. However, some men like to use them for activities such as swimming or jogging.
For more information about the different types of products to manage leaking urine, visit Continence Product Advisor.
Internal male sling
This is a small piece of material (mesh) that presses gently on your urethra and supports the urinary sphincter to keep it closed. This helps to stop urine leaking. You’ll have an operation to fit the sling. It should be tight enough to stop urine leaking out, but loose enough to let you urinate when you want to.
Assess your risk
It’s the most common cancer in men, but most men with early prostate cancer don’t have symptoms. Prostate cancer is not always life-threatening. But when it is, the earlier you catch it the more likely it is to be cured. Answer three quick questions to check your risk. If you’re a trans woman or non-binary, your risk may be different – read our information for trans or non-binary people instead.
You may also like ...

